Gastric sleeve är det andra namnet på denna operation. Den började utföras år 1988, då som öppen kirurgi och som led i en större tarmomkoppling vid svår obesitas (man gjorde s.k. biliopankreatisk diversion med duodenal switch). I slutet på 1990-talet börjades sleeve gastrektomi (SG) göras laparoskopiskt (med titthålsteknik) och efter millennieskiftet insåg man alltmer att en sleeve ”ensamt” utan efterföljande tarmomkoppling stod sig väl för effektiv viktnedgång. Efter detta fick gastric sleeve snabbt en stigande popularitet och är idag den i världen vanligaste fetmaoperationen, i Sverige utgjorde den år 2018 45% av alla obesitasoperationer.
Varför blev sleeve gastrektomi snabbt så populär? Ja den är dels lättare för en kirurg att lära sig (man slipper tarmomkopplingarna vid en gastric bypassoperation), den uppfattas som ”snällare” än bypass med mindre risk för dumping och inga postoperativa tarmvred.
Gastric sleeves verkningsmekanismer
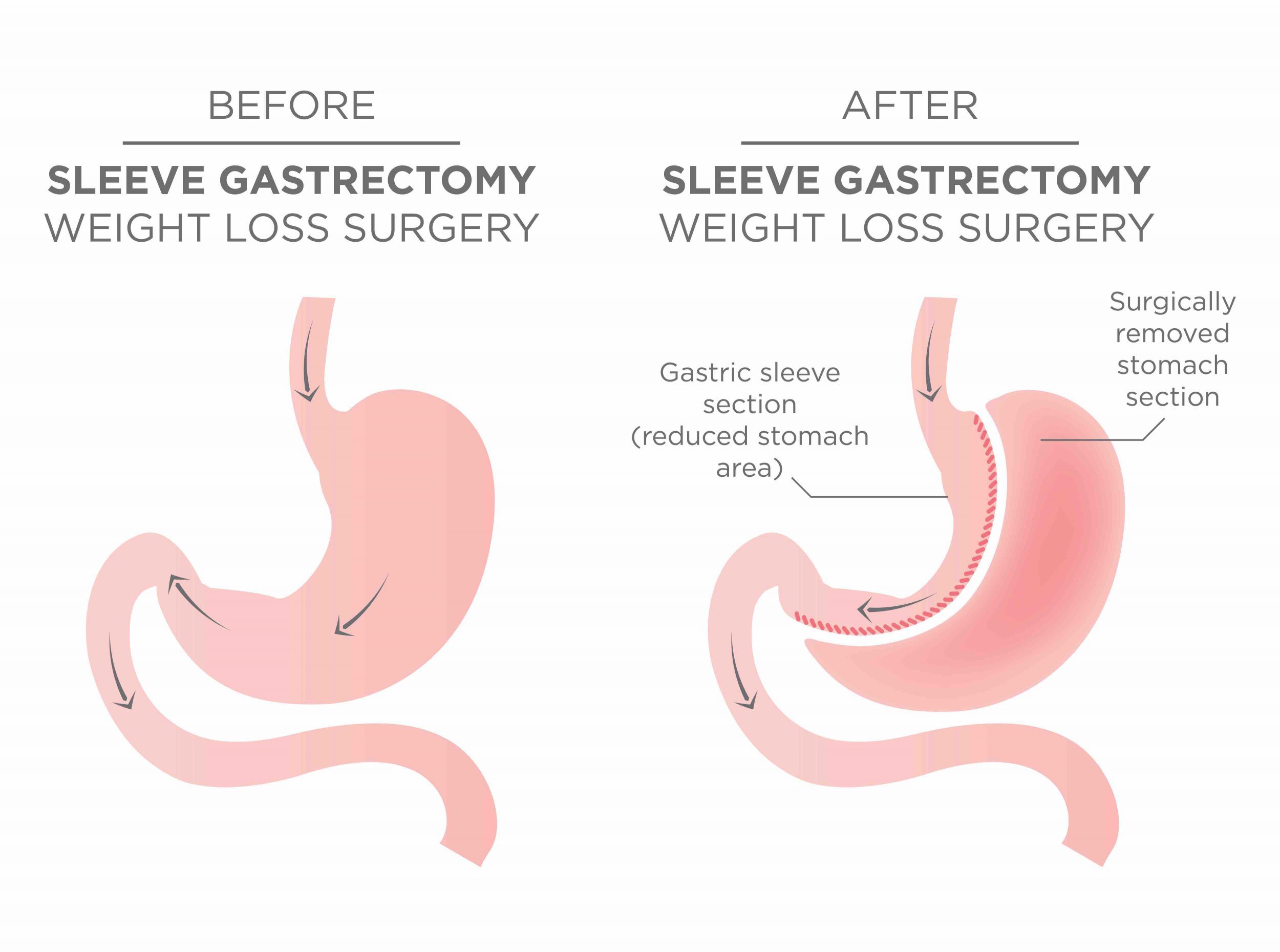
Hur fungerar då en sleeve? Den är en magsäcksoperation, där man opererar bort 85% av magen (man tar bort ”ytterkurvan” på magsäcken). Däremot opererar man inte alls på tarmen. Bortopererad del av magsäcken tas ut ur kroppen. Verkningsmekanismerna är flera: i början märker man tydligt av det restriktiva, alltså att magsäcken är väldigt liten och begränsande. På sikt är däremot effekten på våra hungerhormoner det centrala; precis som vid gastric bypass sänker en gastric sleeve vår ”set point” för vikt i hjärnstammen till mera normala nivåer. De dagliga rutinerna som krävs efter en SG är desamma som efter en bypass -man måste anpassa sig till den nya anatomin i magen, samt vad man nu tål eller inte tål att äta och dricka: 5-6 små måltider per dag, minst 1,5 L vatten per dag, vara fysiskt aktiv samt ta dagliga vitamintillskott.
Sleeve gastrektomins för- och nackdelar
Detta är en utmärkt operation, liksom bypass har den för- och nackdelar. Det har funnits en del missuppfattningar kring sleeve gastrektomi; ibland har den beskrivits som att ”kunna äta upp kakan och ändå ha den kvar” (d.v.s. få effektiv viktnedgång utan att behöva anstränga sig så mycket, slippa dumpingrisk och inte behöva ta vitaminer) vilket definitivt är felaktigt: en sleeveopererad behöver sköta sina dagliga rutiner på exakt samma sätt som en bypassopererad. Exakt när en sleeve är det bästa att välja vet vi inte (det är därför GB Obesitas är med i BEST -studien). Men följande har varit vår uppfattning utifrån kliniska erfarenheter hittills:
Gastric sleeve ger ingen tarmvredsrisk, till skillnad från gastric bypass. Man blir generellt inte lika dumpningskänslig (vilket ju är lite på gott och ont, en del patienter tycker om att de kan dumpa ibland). Vitaminupptaget är försämrat, men sannolikt mindre uttalat så än efter en bypass.
Nackdelarna är risk för försämrade refluxbesvär (halsbränna, sura uppstötningar) samt oklar långtidseffekt på vikten. Operationen går inte heller att återställa till normal anatomi. Däremot kan en sleeve vid behov (oftast p.g.a. viktuppgång) förstärkas med ytterligare en operation: den kan göras om till en gastric bypass eller en SASI.
Kommer sleeve gastrektomi fortsatt att vara världens vanligaste obesitasoperation om 10 år? Det får framtiden -och BEST -studien -utvisa. Följ oss!







Senaste kommentarerna