
Det har gjorts många försök genom åren att behandla fetmasjukdom med mediciner, men de effektiva har hela tiden haft farliga biverkningar. En översikt i BMC Medicine listar åtminstone 25 stycken sedan 1950-talet som fått dras in; exempel som även funnits i Sverige inkluderar Reductil och Acomplia. Kvar fanns bara läkemedlet Orlistat som är begränsat effektivt, samt Mysimba. Det verkade länge som att aptitreglering var alltför central för kroppen för att man skulle kunna ”komma åt” den utan svåra biverkningar.
GLP-1 historiskt
Detta ändrades när man började behandla diabetes med läkemedel som aktiverar receptorn för GLP-1 (glukagonlik peptid-1). GLP-1 produceras naturligt i hormonproducerande celler i tarmslemhinnan. GLP-1 bidrar till att kontrollera glukosnivåerna i blodet i samband med måltid. Normalt sett är halveringstiden bara ett par minuter, men nu lyckades man forska fram molekyler som stannar längre i kroppen. I Sverige godkändes GLP-1-läkemedlet Victoza (liraglutid) mot typ 2 diabetes år 2009.
Man upptäckte snart att dessa mediciner även gav aptitsänkning och viktnedgång hos patienterna, särskilt om man gav lite högre styrka. Victoza följdes då upp av Saxenda, som är liraglutid men i högre styrka med indikation obesitas. Den godkändes i Sverige 2015 och innebär en injektion under huden en gång per dag. I studier ger Saxenda en viktnedgång på 8% av totala kroppsvikten, med oftast övergående biverkningar.
Ozempic -idag världens mest omtalade medicin
Med start 2012 började danska Novo Nordisk utveckla semaglutid, ett GLP-1 läkemedel som är effektivare än liraglutid och samtidigt kan ges en gång i veckan istället för varje dag. År 2017 godkände USA semaglutid för typ 2 diabetes med namnet Ozempic och år 2021 kom versionen mot obesitas, Wegovy. Medieuppmärksamheten (med bl.a. Hollywoodstjärnor i spetsen) exploderade och efterfrågan likaså. I Sverige komplicerades bilden av att Ozempic kom med indikation typ 2 diabetes och läkemedelsförmån -samtidigt som obesitasvarianten Wegovy inte kom hit och oavsett inte hade förmån. Detta har lett till debatt då tillgången på doser Ozempic varit begränsad. En paradoxal konsekvens har också blivit att patienter med obesitas och typ 2 diabetes får medicin med förmån, medan de med ”bara” obesitas får betala hela kostnaden själv(!).
Mounjaro -GLP-1 plus GIP
Amerikanska Eli Lilly utvecklade samtidigt tirzepatid, som verkar på två receptorer i kroppen: GLP-1 och GIP. GIP (gastric inhibitory peptide) är även det ett kroppseget hormon från celler i tarmen. GIP liknar GLP-1 genom att minska matintaget och sänka kroppsvikten (samt vara bra vid typ 2 diabetes). Dessutom har GIP positiva effekter på vår fettväv. Tirzepatid lanserades 2022 som Mounjaro mot typ 2 diabetes och obesitas; läkemedlet kom hit till Sverige hösten 2024. Det är en spruta per vecka och liksom med Saxenda och Wegovy skrivs Mounjaro ut på vanligt recept -men saknar läkemedelsförmån. Man måste alltså betala hela medicinkostnaden själv. (Eli Lilly har sökt förmån i Sverige på indikation typ 2 diabetes, besked väntas i vår.)
Hur effektiva är medicinerna?
I studier går man ner i snitt 15% av sin kroppsvikt med Wegovy (STEP-studierna) respektive drygt 20% med Mounjaro (SURMOUNT-studierna). Det motsvarar att en person som väger 120 kg går ner 18 respektive 24 kg. Vissa går ner mindre, andra mer. Viktigt att komma ihåg är detta: resultaten kommer från stora, välfinansierade studier med utvalda säkert högmotiverade försökspersoner. Dessa fick mycket intensiv livsstilscoachning (i STEP 3 besök hos dietist varannan vecka i 68 veckor, i SURMOUNT 1 nio coach-/dietistbesök under 72 veckor. I bägge fallen träning 150-200 minuter varje vecka, ofta med loggning av träning och livsstil).
Det är alltså läkemedel PLUS strukturerad relativt ambitiös livsstilsändring som ger 15-20% viktnedgång –inte läkemedlet ensamt. Behandlingen är med hög sannolikhet kontinuerlig: du måste fortsätta även efter att du nått din lägsta vikt, annars kommer du att gå upp igen. Detta gör tyvärr priset till en faktor, exempelvis kostar Mounjaro 2650 – 3700 kr per månad.
GLP-1 läkemedel eller operation vid obesitas?
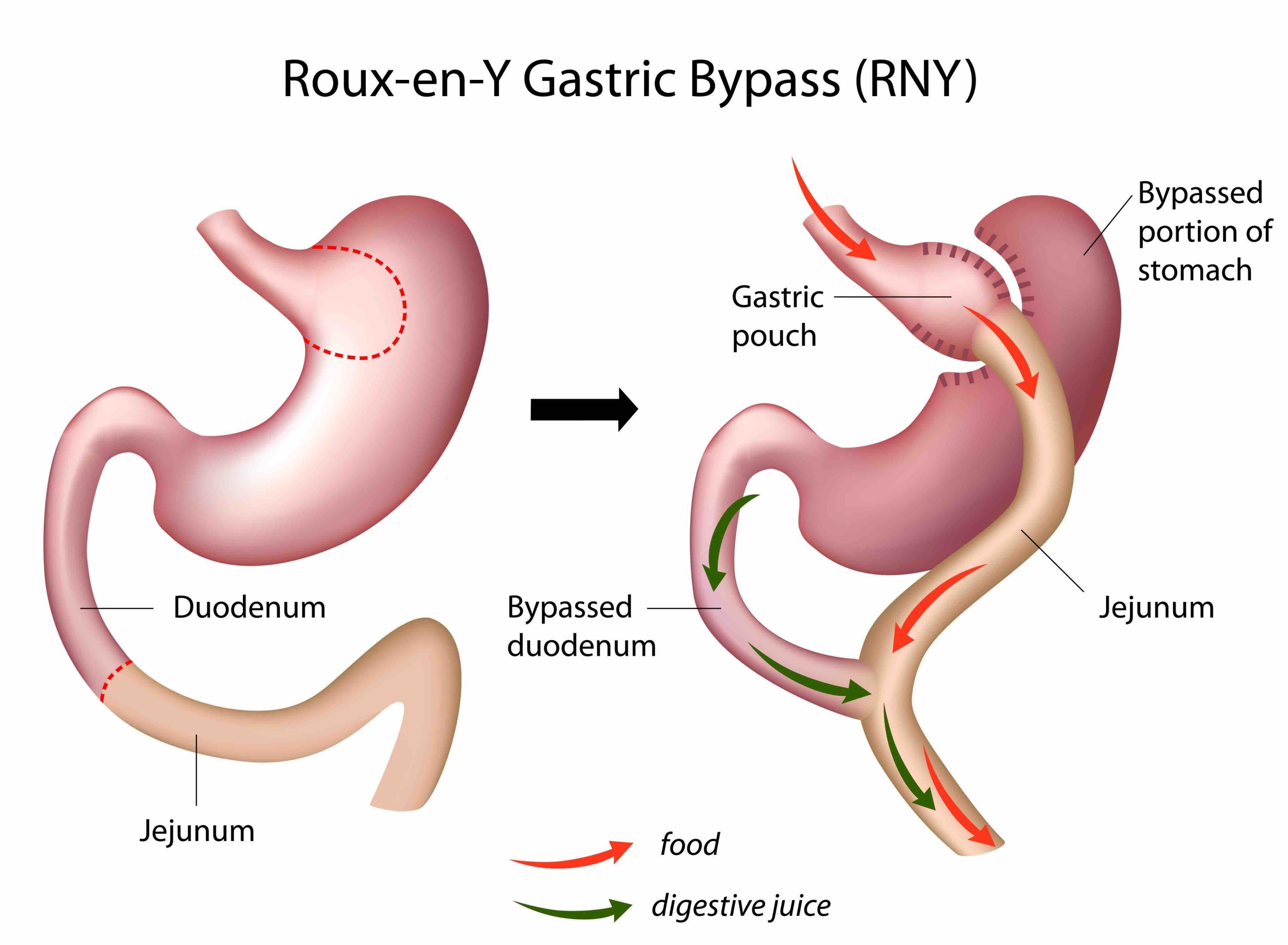
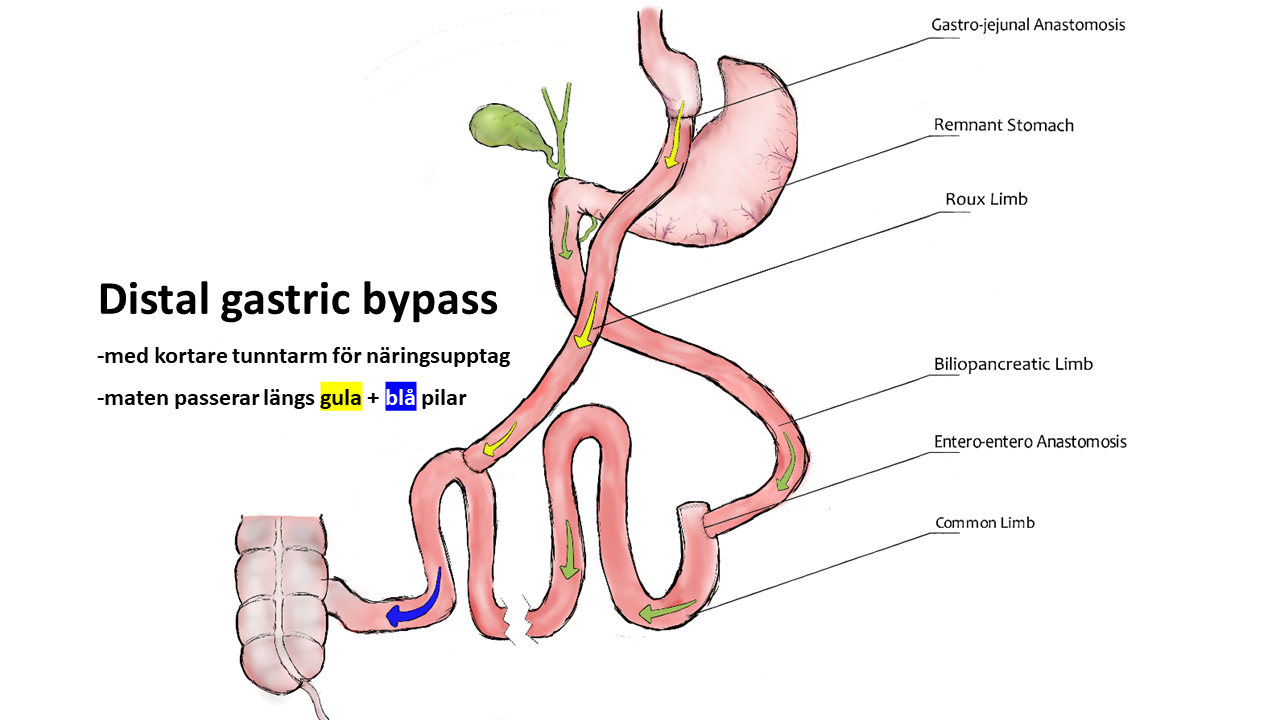
Mekanismerna bakom viktnedgång med modern medicin respektive operation är i grunden desamma: hjärnans set point för kroppsvikt sänks genom att signaleringen till bl.a. aptitcentra i hjärnstammen ändras. Studier har t.ex. visat att en gastric bypass ger tydligt ökade nivåer av såväl GLP-1 som GIP (samma hormonreceptorer som Mounjaro verkar på).
Fördelar med läkemedel är att man slipper operera sig, man kan ”testa” behandling och direkt avbryta om man ångrar sig. Nackdelar är (ofta övergående) magtarmbiverkningar, vissa svarar inte med tillräcklig viktnedgång och effekten kan avta över tid (så kallad takyfylaxi). Då obesitas är en kronisk sjukdom är behandlingen troligen livslång och kostnaden är i nuläget 30000 – 45000 kr per år.
Att det äntligen kommer läkemedel som är effektiva samt har begränsade biverkningar är välkommet. För många patienter har steget från enbart kost och träning direkt till kirurgi varit alldeles för stort, samtidigt som ett ”mellansteg” har saknats. Medicinerna kommer också att öka intresset för obesitas som sjukdom inom allmänna sjukvården (nu blir obesitas mer en sjukdom som ”alla andra”).
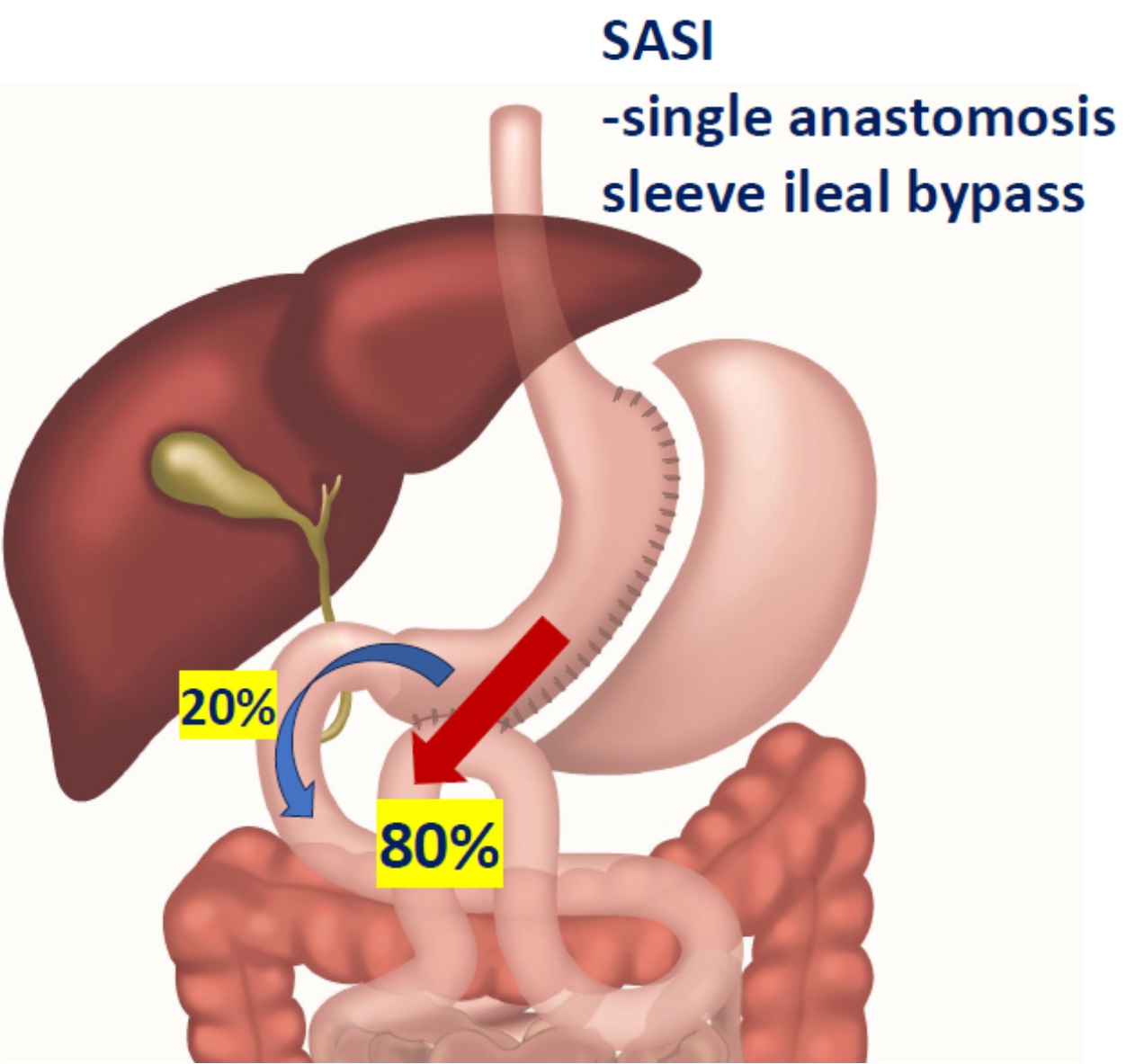
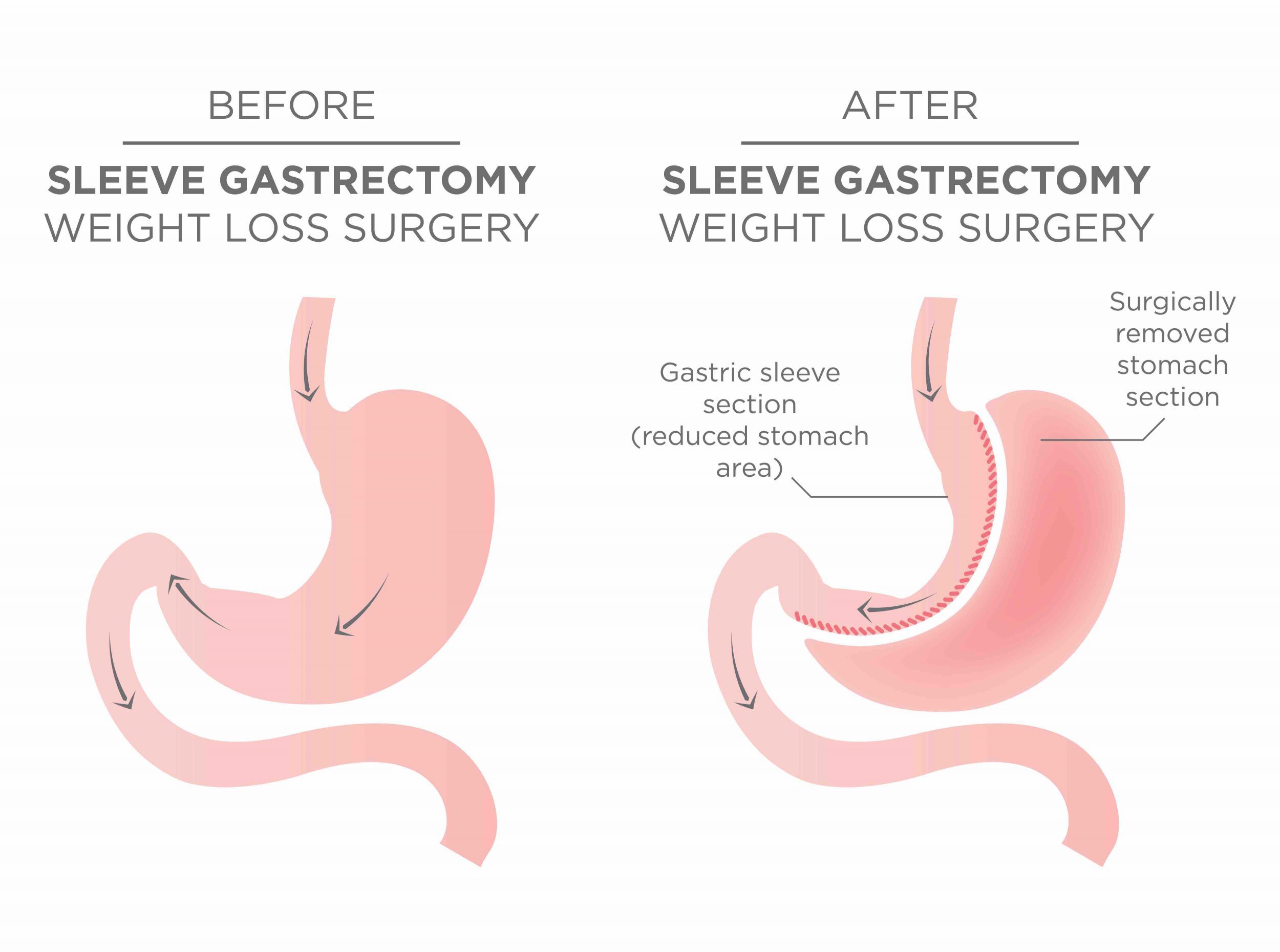
Fördelar med en operation som gastric bypass eller sleeve är potentiellt livslång effekt av en enda behandling, där en sleeveopererad i snitt tappar 26% och en bypass 32,5% av kroppsvikten (en SASI tappar 42%). Nackdelar är att en operation har 3-4% risk för komplikation under läkningen. Man behöver också ändra sina matvanor samt får ett livslångt behov av vitamintillskott och labkontroller.
Vad ska jag välja för behandling?
Med det vi vet idag så är kirurgin mest effektiv och bäst beprövad vad avser långtidsresultat och biverkningar. Det betyder naturligtvis inte att alla vare sig vill eller ska opereras. GLP-1-läkemedel är ett bra komplement till kirurgin och kan tänkas komma in såväl före (lägre BMI), istället för (vill/kan ej opereras) som efter en operation (vid viktrecidiv, s.k. weight regain). Då läkemedel ger 15-20% viktnedgång medan kirurgi ger 26-33-42% så kommer medicinerna att ha bäst effekt vid BMI kring 30-35, högre BMI talar starkt för operation.
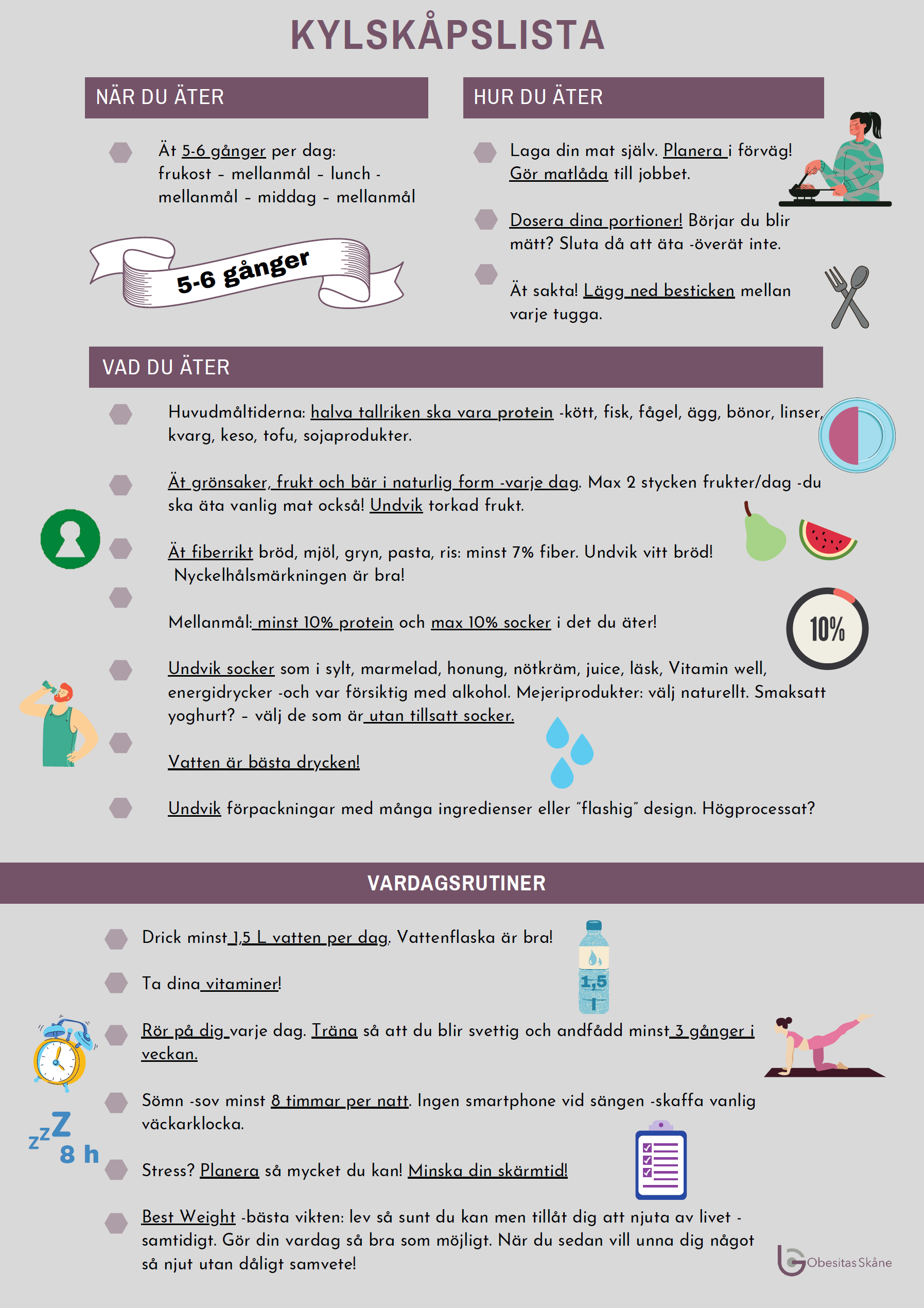
KOM IHÅG: det är en hälsosam livsstil som är grunden här. Varken läkemedel eller operation kommer att ge en bestående viktnedgång ensamt. Använd gärna vår Kylskåpslista om du vill ha ett stöd i vardagen.
Vill Du veta mer? Kontakta oss eller håll utkik efter nästa öppna infomöte online! Om du vill fördjupa dig kring GLP-1 kan vi tipsa om en superintressant djupintervju (på engelska) om att behandlas med Ozempic här (oroa er inte över titeln på podcasten, det är bara clickbait).
Vid tangentbordet -Carl-Magnus














Senaste kommentarerna