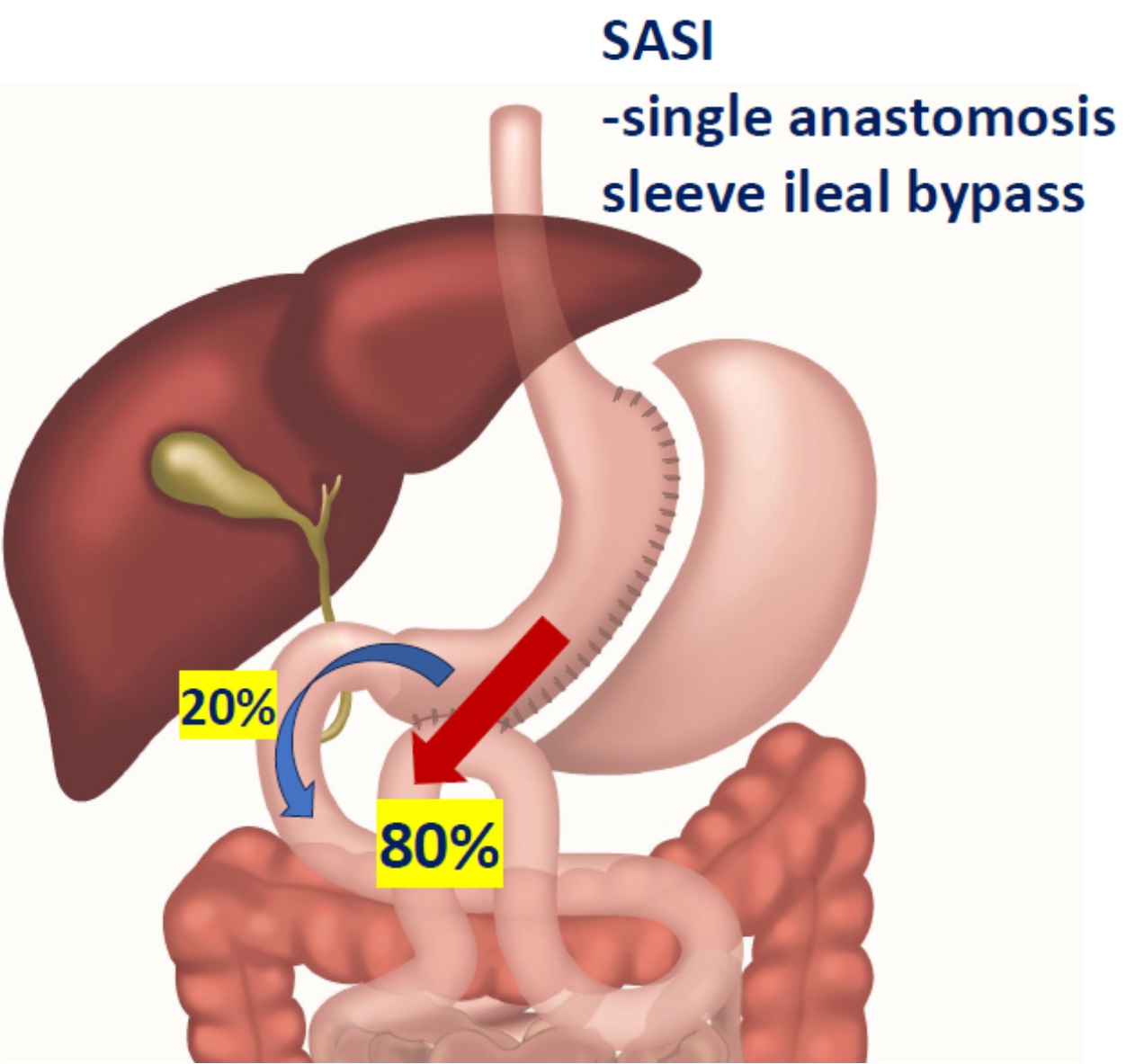
SASI -single anastomosis sleeve ileal bypass
SASI -operationen har beskrivits i vetenskapliga artiklar sedan år 2014. En SASI är till hälften en ”vanlig” gastric sleeve, där man opererar bort ytterkurvan på magsäcken. Därigenom får man dels mindre magsäck, dels lägre produktion av svälthormoner. Vid en sleeveoperation slutar man där. Vid en SASI gör man dessutom en s.k. loopanastomos, där sidan på tunntarmen längre ned i magtarmkanalen kopplas upp mot sleevemagen. Nu kan maten passera ut genom magsäcken via två olika vägar -den normala via nedre magmunnen ut i tolvfingertarmen, eller genvägen ned i den påkopplade tunntarmen.
Verkningsmekanismer hos en SASI
Tillägget av tarmkopplingen vid en SASI ger flera fördelar jämfört med en gastric sleeve: cirka 80% av födan kommer att ta vägen direkt ned i den påkopplade tunntarmen (se bilden ovan). Detta resulterar i stimulering av hormoner som sänker hjärnans set point för kroppvikt (t.ex. GLP-1 och PYY). Därmed får operationen effekter som liknar gastric bypass och en SASI ger också bättre viktnedgång än en gastric sleeve. Att 20% av maten går den normala vägen ut i tolvfingertarmen är bra för vitaminupptaget och blodsockerkontrollen, vilket ger SASI en fördel mot gastric bypass (där ju tolvfingertarmen kopplas förbi helt).
Vad säger forskningen om SASI?
Vårt kirurgteam lett av dr Hjörtur Gislason publicerade år 2023 en studie på 366 patienter opererade med SASI. Man har följt dessa patienter i fyra år efter operationen. Komplikationsrisken var 2,5% första 30 dagarna och 4,6% på lång sikt. Detta är i nivå med riskerna vid bypass eller sleeve. En fördel mot gastric bypass var klart mindre risk för tarmvred. Vinsterna var många: patienterna gick ner i snitt 93% av sin övervikt (eller 41% av sin totala kroppsvikt) -detta är bättre än vid både gastric bypass och sleeve. Tidigare typ 2 diabetes botades hos 93%, högt blodtryck hos 73% och sömnapnesyndrom hos 79%. Vårt team har nu en pågående studie tillsammans med Region Skåne där patienter lottas mellan gastric bypass och SASI för att bättre kunna jämföra effekterna hos de båda metoderna.
Vem kan få en SASI idag?
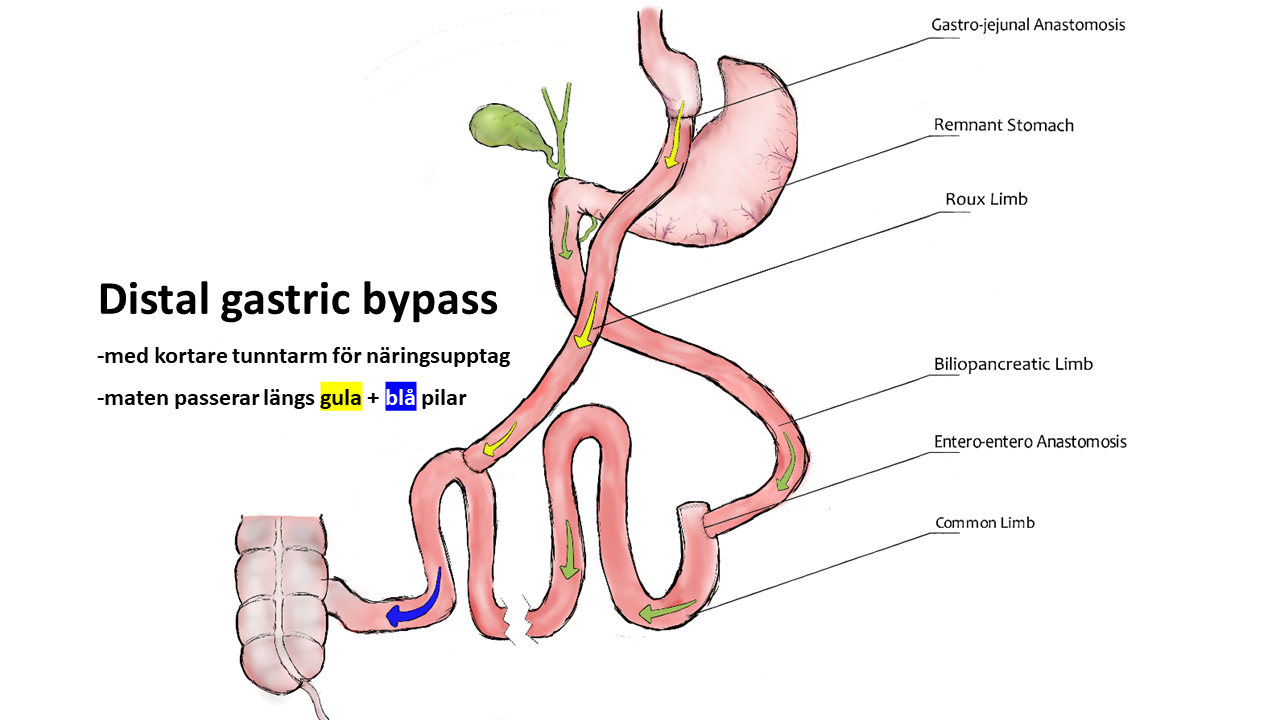
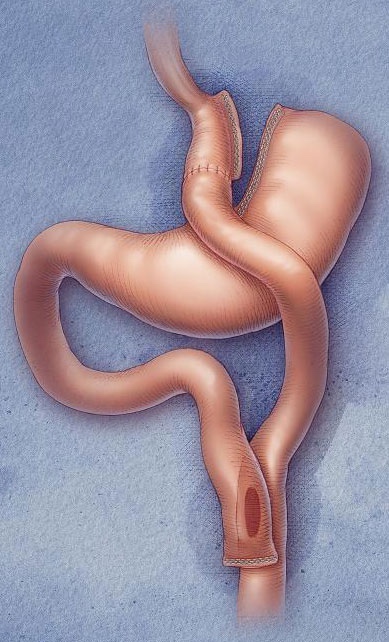
GB Obesitas erbjuder SASI som privatbetald operation redan idag. Lämpliga är t.ex. de som funderat på en sleeve men vill ha en effektivare operation eller de som vill ha något lika effektivt som gastric bypass men med lägre risk för tarmvred och blodsockersvängningar. I utvalda fall (kontakta oss för diskussion!) kan en SASI även vara en behandling av viktuppgång efter tidigare vanlig sleeve. (Alternativet vid weight regain efter sleeve är annars vår operation distal gastric bypass.)
Om en SASI inte skulle fungera av något skäl, så kan den göras om till en vanlig sleeve eller opereras om till en gastric bypass.





Senaste kommentarerna